Inherited diseases
Most inherited diseases are caused by recessive alleles. These are the mutant forms of normal alleles found in healthy people. A mutation is a change in the DNA base sequence, changing or preventing the production of the protein, which the gene normally codes for. Diseases caused by mutations are often referred to as inherited diseases. They are different from infectious diseases which are caused by microbes.
Sickle Cell Anaemia
Sickle cell anaemia is an inherited disease of the blood. The red blood cells in the sufferers of this disease form an S-shape like a sickle which causes anaemia and hence the name. The disease is common in people of African descent and is also common in Pakistan and India.
In order to explain sickle cell anaemia an understanding of the function of haemoglobin is required. Haemoglobin is an iron rich protein in the red blood cells which enables the blood cells to carry oxygen from the lungs to other parts of the body. When red blood cells pass through the lungs the haemoglobin takes in oxygen and releases carbon dioxide it has collected in a process called oxygenation. On leaving the lungs the haemoglobin in the red blood cells delivers the oxygen to the tissues in the body and removes the excess carbon dioxide in a process called deoxygenation. During deoxygenation the haemoglobin molecules smoothly rearrange themselves into a different shape.
In sickle cell anaemia the smooth rearrangement of the haemoglobin does not occur. As mentioned earlier haemoglobin is an iron rich protein. Proteins are made up of chains of amino acids. The type and sequence of the amino acid determine the type of protein. The production of protein, or protein synthesis, is controlled by DNA. The code for creating protein comes from the genes with each gene carrying a specific code or set of instructions for making a specific protein. Sickle cell anaemia is caused by a mutation to the gene that code for the production of haemoglobin in the red blood cells. The gene is situated on chromosome 11.
The diagram below shows the difference in the synthesis of haemoglobin in normal DNA and mutated DNA in sickle cell anaemia.
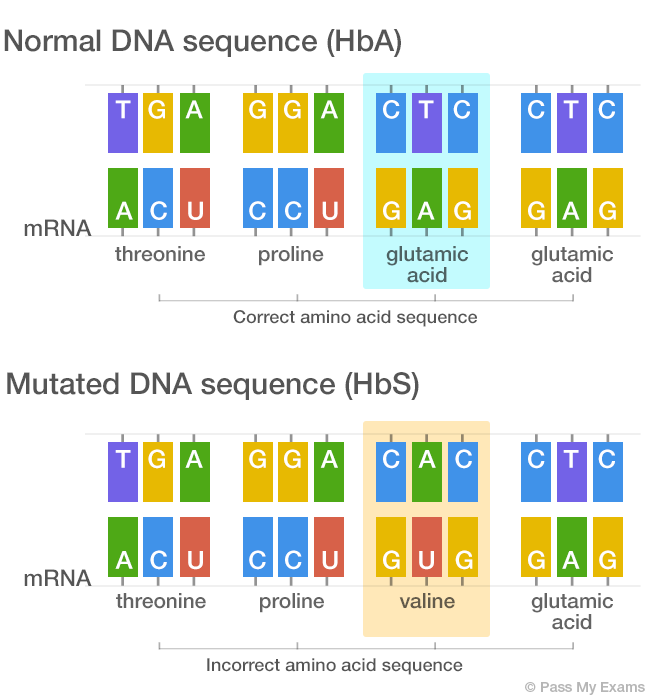
In the mutated DNA sequence the Thymine (T) is replaced by Adenine (A) in the second position of the triplet. This type of mutation is called a substitution. The change in base sequence of the DNA results in a codon of the mRNA being altered during transcription. This fault results in a different amino acid (Valine) being inserted into the protein chain during translation. The presence of valine in the protein makes the deoxygenated haemoglobin less soluble. So when haemoglobin losses its oxygen the molecules come out of solution and crystallise into rod like structures. This distorts the normal circular shape of the red blood cell, causing them to a take a rigid, sickle shape.
The primary symptoms of the disease are anaemia (lack of haemoglobin) and the tendency for the red blood cells to change shape rendering them useless. The sickle cells have a tendency to jam in capillaries and small blood vessels preventing normal blood flow as show in the image below.
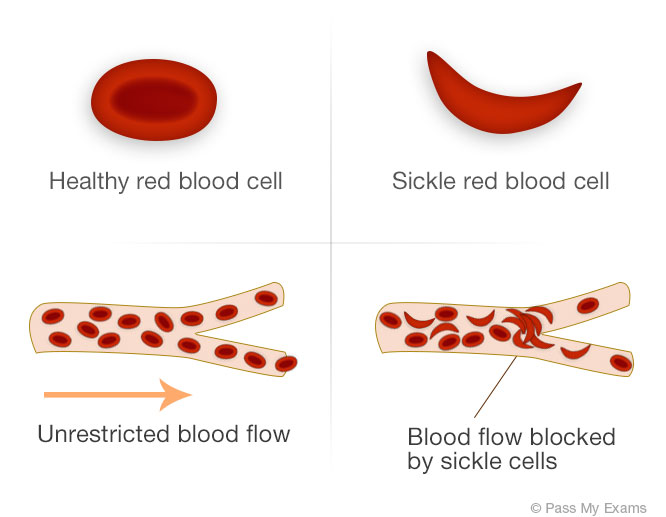
The blocking of the blood vessels results in secondary symptoms such as severe pain to the arms, leg, back and stomach. Joints can become stiff and hands and feet may swell. Individual suffering from sickle cell anaemia may show poor signs of growth and development and are prone to infections and strokes.
There is currently no cure for sickle cell anaemia so most treatments aim to treat individual symptoms of the disease. Treatment plans involve a number of different health care professionals working together such as a haematologist (specialist in blood disorders), a clinical psychologist, a physiotherapist, a dietician and specialist nurse. Regular blood transfusions are used to help reduce the risks of strokes. This also involves chelation treatment afterwards to remove excess iron from the patient’s body. Excess iron in the body can lead to complications including liver cancer, diabetes and infections. Chelation therapy is a medical procedure in which a chemical is injected into the body which binds to heavy metals such as iron and mercury in the blood so that it can be excreted via the urine. For young children daily antibiotics, such as penicillin, are often given to protect against infections. Prolonged episodes of pain are referred to sickle cell crisis. If this is recurring and patients are not responding from other treatments Hydroxylcarbamide is recommended. This medication stimulates the production of foetal haemoglobin. Foetal haemoglobin is found in unborn babies and is gradually replaced by adult haemoglobin as the child develops. Foetal haemoglobin is not affected by the sickle cell mutation and to some extent can take over the role of adult haemoglobin. This treatment helps reduce some of the risks associated with sickle cell anaemia. There are some risks and side effects associated with this treatment however in most cases the potential benefits outweigh the risks.
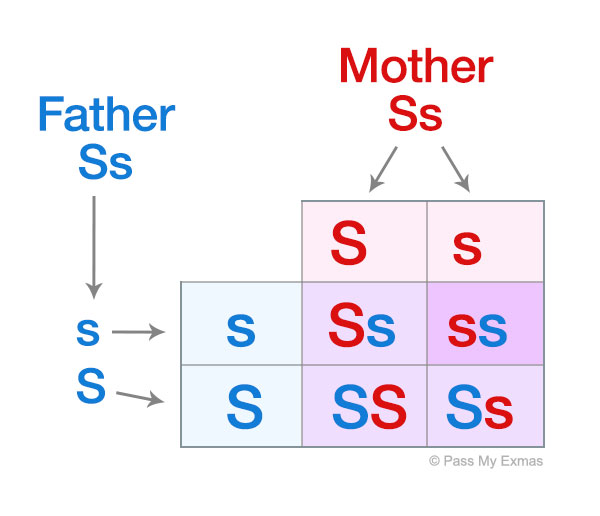
Sickle cell anaemia is caused by a recessive allele, thus to have the disease a person must be homozygous and carry two copies of the recessive allele. If we denote the recessive allele by “s” and the dominant allele by “S”, then a heterozygous person “Ss” does not have the disease but acts as a carrier who can pass it on to their children.
For example, if a father and mother are carriers then the table below shows there is a 1 in 4 chance of their child having sickle cell anaemia.
Sickle cell anaemia and malaria
An interesting point about sickle cell malaria is related to the locations where the disease is so common. The distribution of sickle cell anaemia is across Africa, Pakistan, India and some parts of the Middle East. This also happens to match the areas where malaria is prevalent. Carriers of the faulty gene responsible for sickle cell anaemia are less susceptible to malaria as the malaria parasite multiplies inside normal blood cells. Heterozygous carriers have a selective advantage over non carriers as they are more likely to be resistant to malaria and pass on their genes to the next generation.
Summary of Sickle Cell Anaemia
The table below gives a summary of Sickle cell anaemia:
Cause
- Sickle cell anaemia is caused by a recessive mutation in a gene located on chromosome 11. The gene codes for the protein haemoglobin in the red blood cells which carries oxygen form the lungs to other parts of the body.
- The mutation results in a change in one of the bases in the DNA sequence from an A to a T. This then results in the incorrect amino acid valine instead of glutamic acid being added in the haemoglobin chain.
- This causes the body to produce a new form of haemoglobin (HbS) which behave differently to regular haemoglobin.
- HbS causes the haemoglobin to crystallise into rod like structures when it loses its oxygen. This distorts the normal circular shape of the red blood cell, causing them to a take a rigid, sickle shape.
Symptoms
- Anaemia – a decline in haemoglobin or red blood cells in the blood resulting in a decreased amount of oxygen being transported around the body.
- Stroke, associated with the supply of blood to the brain being blocked due to the sickle shaped cells.
- Acute chest syndrome associated with the sickle shaped cells blocking blood vessels in the lung.
- Pulmonary hypertension associated with sickle shaped red blood cells blocking the blood flow from the lungs to the heart.
- Sever pains to the arms, legs, back and stomach.
- Joint pains.
- Increased risk of infection as sickle cell anaemia can damage the spleen which is a key organ involved in fighting infections.
Treatment
- Regular blood transfusions followed by chelation therapy.
- Hydroxylcarbamide to stimulate the body to produce foetal haemoglobin.
- Daily antibiotics to fight infections.
- Pain killers
- Lifestyle and dietary changes.
